What are White Spots on Gums After Whitening?
Discovering white spots on your gums after teeth whitening can be alarming. These spots, often appearing as small, localized areas of discoloration, can arise due to various factors associated with the whitening process. Understanding the underlying causes is crucial for addressing the issue promptly and effectively. These spots may signal minor irritation or could indicate more significant problems requiring professional dental attention. In this guide, we’ll explore the common reasons behind the appearance of these white spots, helping you understand what’s happening in your mouth and what steps to take.
Chemical Burns from Whitening Products
Understanding the Role of Whitening Agents

Teeth whitening products, whether professional treatments or at-home kits, often contain bleaching agents, such as hydrogen peroxide or carbamide peroxide. These agents work by penetrating the enamel and oxidizing the stains within the tooth structure. While effective in brightening teeth, these chemicals can also cause irritation if they come into contact with the sensitive gum tissues. The concentration of these agents significantly impacts the potential for adverse effects, with higher concentrations increasing the risk of gum irritation and burns.
How Whitening Products Cause Burns
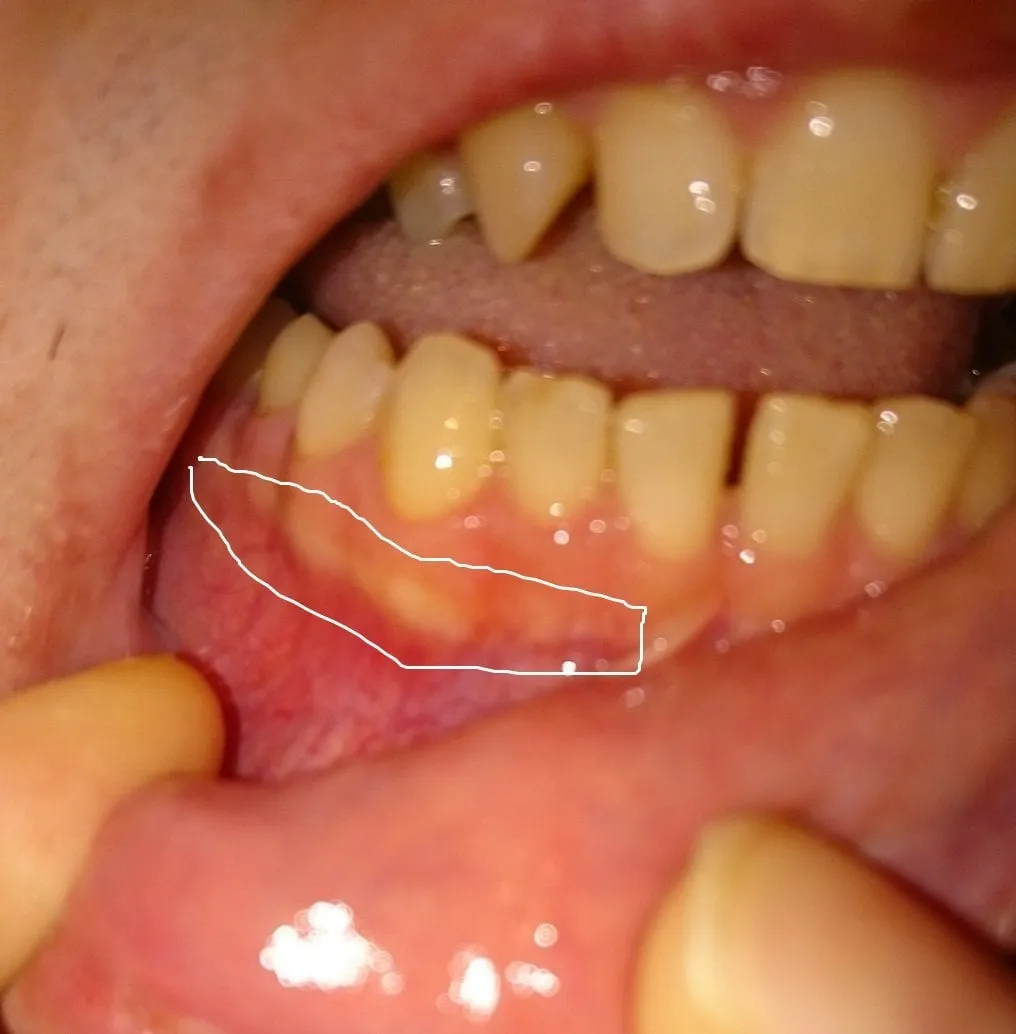
Chemical burns on the gums can occur when the whitening agent comes into direct contact with the gum tissue for an extended period. This often happens if the whitening trays don’t fit properly, allowing the gel to leak, or if excessive amounts of the product are used. The strong chemicals in the whitening agents can irritate the soft tissues of the gums, leading to inflammation, redness, and the characteristic white spots, which represent areas where the surface cells have been affected by the chemical. The severity of the burn depends on the concentration of the whitening agent and the duration of exposure.
Symptoms of Chemical Burns
Recognizing the symptoms of chemical burns on your gums is essential for prompt treatment. Common signs include white or discolored patches on the gums, tenderness, pain, and a burning sensation. The affected areas may also appear swollen or inflamed. In more severe cases, blisters or ulcers can form. If you experience any of these symptoms after teeth whitening, it’s crucial to stop the treatment immediately and consult your dentist.
Preventing Chemical Burns
Preventing chemical burns involves several key steps. When using at-home whitening kits, ensure that the trays fit snugly and don’t allow the gel to leak onto your gums. Always follow the product instructions carefully regarding the amount of gel and the duration of use. If you’re undergoing professional whitening, your dentist will take precautions, such as using a protective barrier to shield your gums. It’s also beneficial to inform your dentist about any gum sensitivities or conditions before the whitening process begins. Careful application and adherence to guidelines can greatly reduce the risk of gum irritation.
Gingival Recession
Causes of Gingival Recession
Gingival recession, or the receding of the gum line, can be caused by several factors, including aggressive brushing, periodontal disease, and genetics. Overly vigorous brushing with a hard-bristled toothbrush can erode the gum tissue over time, exposing the tooth roots. Periodontal disease, caused by bacterial infections, can also lead to gum recession as the supporting tissues of the teeth are damaged. Additionally, some individuals are genetically predisposed to thinner gum tissues, making them more susceptible to recession.
How Whitening Can Exacerbate Recession

Teeth whitening can exacerbate gingival recession in several ways. If the gums are already receding, the whitening agent may come into direct contact with the exposed tooth roots, which are more sensitive than the enamel-covered crowns. This contact can cause irritation and discomfort. Furthermore, the whitening process may increase tooth sensitivity, making the area more vulnerable to external stimuli. Those with existing recession should inform their dentist before whitening to take extra precautions and avoid further irritation.
Treatments for Gingival Recession
Treatment for gingival recession depends on the severity of the condition. For mild recession, your dentist may recommend changes to your oral hygiene routine, such as using a soft-bristled toothbrush and gentle brushing techniques. In more severe cases, surgical procedures like gum grafting may be necessary. Gum grafting involves taking tissue from another part of your mouth (usually the palate) and attaching it to the receding area to restore the gum line. Regular dental check-ups and professional cleanings are also essential for managing and preventing recession.
Enamel Demineralization
The Science Behind Enamel Demineralization

Enamel demineralization occurs when minerals, such as calcium and phosphate, are lost from the tooth enamel. This process is often triggered by acids, which can come from food, drinks, or even the whitening agents themselves. When the enamel loses minerals, it becomes more porous and susceptible to staining and sensitivity. The process is reversible in its early stages, but if left unchecked, it can lead to tooth decay and structural damage. The balance between demineralization and remineralization is key to maintaining healthy teeth.
Why Whitening Can Lead to Demineralization
Whitening agents, particularly those containing hydrogen peroxide, can contribute to enamel demineralization. The bleaching process involves chemical reactions that can temporarily weaken the enamel structure. The porous nature of demineralized enamel can also make it appear whiter, which can sometimes be mistaken for the intended whitening effect. This effect is more pronounced with higher concentrations of whitening agents or when the treatment is prolonged. Therefore, following your dentist’s recommendations and using products as directed is essential to minimize the risk of demineralization.
Remineralization Strategies
Fortunately, enamel demineralization can be reversed through remineralization. This involves restoring the minerals to the enamel. Using fluoride-containing toothpaste and mouthwash is a common and effective way to promote remineralization. Fluoride helps to strengthen the enamel and make it more resistant to acid attacks. Dietary changes, such as reducing the intake of sugary and acidic foods and drinks, can also support the remineralization process. Your dentist may also recommend professional fluoride treatments or other products to aid in remineralizing your teeth.
Ulcers and Irritation

Common Irritants and Their Impact
The oral cavity is constantly exposed to various irritants that can lead to ulcers and irritation. These irritants can include spicy foods, acidic beverages, and certain ingredients in toothpaste or mouthwash. Mechanical irritation from brushing, dental work, or sharp edges on teeth can also cause ulcers. These irritants disrupt the delicate balance of the oral tissues, leading to inflammation and, in some cases, the formation of painful sores or ulcers.
How Whitening Triggers Ulcers
Teeth whitening can trigger ulcers in several ways. The strong chemicals in whitening agents can irritate the sensitive tissues of the mouth, leading to inflammation and the development of ulcers. If the whitening product comes into contact with any existing minor cuts or abrasions, it can exacerbate the irritation, making the area more susceptible to ulcer formation. Additionally, the increased sensitivity that some people experience after whitening can make them more aware of any minor irritations, potentially leading to the perception of ulcers.
Treatment and Relief of Ulcers

The treatment for ulcers caused by whitening involves several strategies to provide relief and promote healing. Avoiding irritating foods and drinks, such as spicy or acidic items, is crucial. Using a gentle toothpaste and rinsing with warm salt water can also help soothe the irritated tissues. Over-the-counter pain relievers may be used to manage discomfort. In severe cases, your dentist might prescribe topical medications to speed up the healing process. Practicing good oral hygiene is essential to prevent secondary infections and promote faster recovery.
Allergic Reactions
Identifying Allergic Reactions to Whitening Agents
Allergic reactions to teeth whitening products are less common but can occur. These reactions can manifest in various ways, including white spots, swelling, and irritation of the gums and surrounding tissues. The most common allergens in whitening products are the bleaching agents themselves (such as hydrogen peroxide or carbamide peroxide) or other additives in the formula. Identifying an allergic reaction involves recognizing the symptoms and assessing whether they appeared after using a whitening product.
Symptoms of Allergic Reactions
Symptoms of an allergic reaction to teeth whitening can vary in severity. Mild reactions may involve itching, redness, or a tingling sensation in the gums or mouth. More severe reactions can include swelling of the lips, tongue, or face, difficulty breathing, and the formation of blisters or sores. In rare cases, severe allergic reactions can lead to anaphylaxis, a life-threatening condition requiring immediate medical attention. If you experience any of these symptoms, it is important to stop using the product and consult with your dentist or physician.
Seeking Medical Attention
If you suspect that you are experiencing an allergic reaction to a teeth whitening product, it is crucial to seek medical attention promptly. Mild symptoms may be addressed by stopping the use of the product and consulting with your dentist. However, if you experience more severe symptoms, such as difficulty breathing, swelling, or any other signs of anaphylaxis, seek immediate medical help. Your doctor can provide appropriate treatment and assess the severity of the reaction, helping to prevent any serious complications.
Other Potential Causes
Fungal Infections
Fungal infections, such as oral thrush, can sometimes manifest as white spots or patches on the gums. These infections are often caused by an overgrowth of Candida albicans, a type of yeast that naturally occurs in the mouth. Factors that can increase the risk of oral thrush include weakened immune systems, antibiotic use, and the use of dentures. If you notice white patches that are thick and can be wiped away, it’s essential to see a dentist to confirm a diagnosis and receive appropriate treatment.
Bacterial Infections
Bacterial infections can also lead to white spots or lesions in the mouth. These infections may arise from poor oral hygiene, trauma, or underlying health conditions. They can cause inflammation, pain, and the formation of white spots or ulcers on the gums. If you suspect a bacterial infection, consult your dentist for diagnosis and treatment. Treatment usually involves antibiotics and may include scaling and root planing to remove bacteria and infection.
What to Do If You See White Spots
Consulting a Dentist
If you notice white spots on your gums after whitening, the first step is to consult with your dentist. They can properly diagnose the cause of the spots and recommend the appropriate course of action. Your dentist will examine your gums and teeth, ask about your whitening process, and evaluate any other relevant symptoms. They can provide a professional assessment and suggest treatment options to address the issue effectively. Early diagnosis and treatment are crucial to prevent any potential complications.
Follow-Up Care and Maintenance
Follow-up care and maintenance are essential for ensuring your gum health and preventing future issues after teeth whitening. Depending on the cause of the white spots, your dentist may recommend specific treatments, such as topical medications, changes to your oral hygiene routine, or additional dental procedures. Regular check-ups and professional cleanings will also help to monitor your oral health and address any potential problems early on. Maintaining good oral hygiene practices, including brushing twice a day and flossing daily, is crucial for long-term oral health.
